Welcome to Infinite Medical Billing Solutions—Your Trusted Medical Billing Company
We work with healthcare providers throughout the United States as a medical billing outsourcing company. Our services include medical billing and coding services for both medical professionals and laboratories. Experienced and trustworthy, we are dedicated to giving our clients premium service that benefits them and their customers.
Our Services
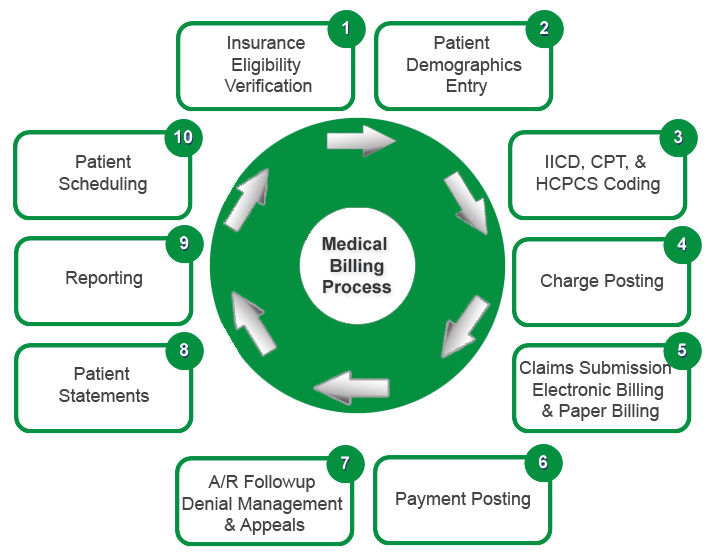
Medical Billing Process
We maintain the great level of confidentiality with all the information that your practice provides us. It’s our promise to provide the highest quality service to you client. We always listen to your concerns, understand your concerns, ask the right question if there will be any confusion and reached your exact goal and objects. Here are few medical billing specialties
Our Specialties